
Webinar: What is a Clinical Trial and Why Should I be Involved?
What is a Clinical Trial and Why Should I be Involved?
Clinical Trials is a priority area for WPA as they are critical for driving medical progress, improving patient outcomes, and shaping the future of healthcare. They provide the foundation for evidence-based medicine, personalized treatments, and the development of innovative therapies that can positively impact the lives of patients worldwide.
The theme of Word Patients Safety Day (WPSD) 2023 is “Engaging patients for patient safety". Considering this theme, the WPA organized a Webinar on the clinical trial titled: ‘’What is a Clinical Trial and Why Should I be Involved?’’ on 5th September from 11:00 am to 12:00 pm (EST).
WPA invited prominent patient safety champions and health care experts who shared their insights on the topic with a large online audience. A report and full video recording of the event are shared below.
What are Clinical Trials?
Professor Dr. Sean Mackey, MD, PhD | Stanford University, USA
A distinguished expert from Stanford University, Professor Dr. Sean Mackey’s presentation on clinical trials provided valuable insights into the world of medical research. It illuminated the significance of clinical trials, their meticulous process, and the potential advantages and disadvantages for individuals. With this knowledge, individuals can make informed decisions about whether to participate in clinical trials, contributing to both their own healthcare journey and the advancement of medical science. Dr. Mackey initiated the presentation by defining clinical trials as controlled research studies designed to evaluate new medical treatments, interventions, or therapies. He emphasized the crucial role of clinical trials in assessing the safety and efficacy of new treatments before they become available to the general public. Dr. Mackey elaborated on the rigorous process of conducting clinical trials, which typically involves several phases, including pre-clinical testing, phase I (safety), phase II (efficacy), and phase III (large-scale efficacy) trials. He highlighted the importance of stringent protocols, ethical considerations, and informed consent throughout the process. The presentation underscored several potential benefits for individuals participating in clinical trials. Dr. Mackey candidly discussed the risks involved in clinical trials, emphasizing that they are not without potential drawbacks. These risks may include unknown side effects, discomfort, and the possibility of receiving a placebo rather than the experimental treatment. The presentation also delved into the typical activities and procedures involved in clinical trials, such as medical examinations, laboratory tests, treatment administration, and ongoing monitoring to assess treatment efficacy and safety. Dr. Mackey highlighted the diversity of clinical trials, including trials for new drugs, medical devices, behavioral interventions, and prevention strategies. Each type of trial serves a specific purpose in advancing medical knowledge. Lastly, the presentation emphasized the importance of careful consideration before participating in a clinical trial. Dr. Mackey encouraged individuals to consult with their healthcare providers, fully understand the trial’s purpose, potential risks, benefits, and alternatives, and ensure that their decision aligns with their own medical needs and values.
What do I Ask before I Go for Clinical Trials?
Dr. Lembit Rägo, MD, PhD | CIOMS, Switzerland
Dr. Lembit Rägo, representing the Council for International Organizations of Medical Sciences (CIOMS) in Switzerland, delivered a comprehensive presentation titled “What do I ask before I go for a Clinical Trial?" Dr. Rägo began by outlining CIOMS’s mission, emphasizing its dedication to promoting the highest ethical standards in medical research involving humans. This sets the stage for discussing the ethical background of clinical trials. He stressed the ethical justification for conducting health-related research involving humans, which lies in the scientific and social value of such research. The goal of clinical trials, Dr. Rägo explained, is to scientifically assess the safety and efficacy of proposed treatments, prevention strategies, and behavioral approaches.
Dr. Lembit Rägo’s presentation offered a valuable roadmap for individuals considering participation in clinical trials. By posing these essential questions and seeking clear answers, potential participants can make informed decisions that align with their medical needs, values, and expectations. This empowers individuals to contribute to medical research while safeguarding their own well-being.
Dr. Rägo encouraged individuals to inquire about the status and approval of the ethics committee overseeing the trial. Participants should fully understand what informed consent entails. This involves knowing the purpose, risks, and benefits of the trial, as well as their right to withdraw at any time without penalty. Patients should inquire about who is conducting the clinical trial, whether it’s a pharmaceutical company, academic institution, or healthcare provider. Understanding the sponsor’s motives and track record can be essential. Patients with existing medical conditions should ascertain whether they can continue with their current treatments while participating in the trial. Understanding the trial’s purpose, potential benefits, and associated risks is crucial for informed decision-making. Knowing how long the trial will last allows participants to plan their commitments accordingly. Participants should clarify whether they can leave the trial at any time and what consequences, if any, might result from withdrawal. Inquiring about costs and potential compensation is vital to avoid unexpected financial burdens. Patients should ask about post-trial care and whether they will receive continued medical attention after the trial concludes. Understanding the eligibility criteria helps individuals assess if they meet the necessary requirements for participation. Familiarizing oneself with the trial’s design, such as whether it’s a randomized controlled trial or an observational study, provides insight into how data will be collected and interpreted. Patients should know where to access additional information about the trial and if they can connect with other participants for support.
World Health Assembly 2022 Resolution on Clinical Trials
Dr. Vasee Moorthy, MD, MBChB, PhD | World Health Organization
Dr. Vasee Moorthy, MD, MBChB, PhD, a Senior Advisor at the World Health Organization (WHO) Research for Health Department in Switzerland, delivered a presentation on the World Health Assembly’s 2022 resolution concerning clinical trials.
Dr. Moorthy commenced by referencing the World Health Assembly’s call for improvements in clinical trials in May 2022. He elucidated the key features of this resolution, which addressed issues related to transparency, ethics, and the robustness of clinical trials. Dr. Moorthy highlighted WHO’s role in providing guidance on best practices for clinical trials. This guidance aims to enhance the quality of evidence generated from clinical trials and ensure that they meet ethical and scientific standards. He mentioned the intended audience and the availability timeline for this guidance. Dr. Moorthy discussed several factors that could facilitate the resolution of key barriers to clinical trials. These factors include collaboration between stakeholders, transparency in trial data sharing, capacity building in low-resource settings, and ethical oversight. In his presentation’s conclusion, Dr. Moorthy shared an illustration depicting the stages of baseline mapping of clinical trial capabilities and how elements of a self-assessment toolkit emerge from this process. This toolkit can assist organizations and institutions in evaluating and improving their clinical trial practices. Dr. Vasee Moorthy’s presentation shed light on WHO’s commitment to improving the quality of evidence generated from clinical trials. Through the World Health Assembly’s resolution and WHO’s guidance initiatives, the organization aims to address key challenges, promote best practices, and ultimately contribute to better global health outcomes. The development of a self-assessment toolkit underscores WHO’s dedication to assisting stakeholders in the clinical trials ecosystem in achieving higher standards of research excellence.
My Experiences (Barriers & Opportunities) on Clinical Trials
Christin Veasley | Chronic Pain Research Alliance, USA
Christin Veasley’s presentation underscored the critical importance of involving patients in clinical research. By challenging traditional research models and expanding the research team to include patients and various stakeholders, research becomes more patient-centered, relevant, and impactful. This patient-engaged approach not only improves research outcomes but also contributes to enhancing the quality of healthcare and people’s lives.
Veasley began her presentation by outlining the roles of traditional clinical research team members. These roles typically include researchers, clinicians, scientists, and other professionals who design, conduct, and analyze clinical studies. She then addressed the need to challenge the traditional research model by acknowledging that individuals affected by research have the right to influence research topics and methodologies. The principle of “Nothing about us without us" underscores the importance of involving patients in research decision-making processes. For example, patients living with a rare disease may have unique insights into the daily challenges they face, which can inform the design of clinical trials and patient-reported outcome measures. Veasley, then, introduced a paradigm shift in which new members, including patients, doctors, clinicians, medical insurers, and health systems, are integrated into the traditional clinical research team. This expanded team collaboratively shapes the research agenda and methodologies. The presentation emphasized how this change improves clinical research and, consequently, people’s lives. By incorporating diverse perspectives and experiences, research becomes more patient-centered, relevant, and likely to lead to effective interventions. Veasley elaborated on ways in which patient partners contribute to the research team, such as providing input on research questions, assisting in study design, participating in protocol development, and offering valuable insights during data interpretation. The presentation concluded with a powerful message: “Research is better when we do it together." This highlights the transformative impact of collaboration between researchers, clinicians, and patients, resulting in more meaningful research outcomes and improved healthcare.
My Experiences (Barriers & Opportunities) on Clinical Trials
Ruth Nankanja Mukiibi | Sickle Cell Organization, Uganda
Ruth Nankanja Mukiibi, the Executive Director of the Sickle Cell Association of Uganda, delivered a presentation underscoring the pivotal role of strong regulatory systems in healthcare. By sharing her personal experiences and advocating for sickle cell patients, she exemplified the positive impact of patient involvement in regulatory activities. Her insights into overcoming barriers and creating awareness can serve as a valuable guide for patient communities in Africa and beyond, ultimately contributing to better healthcare outcomes and patient-centered policies.
Mukiibi began her presentation by emphasizing the importance of regulatory systems in healthcare, referring to the Global Benchmarking Tool (GBT) by the World Health Organization (WHO). Regulatory systems play a crucial role in ensuring the safety, efficacy, and quality of healthcare products and services. She proceeded to explain how African patients are increasingly engaging in regulatory activities. Patients are now active participants in the decision-making processes related to healthcare regulations, contributing valuable insights and advocating for their needs and interests. Mukiibi shared her personal experience as a member of the technical working committee for non-communicable diseases in the Ministry of Health (MoH) in Uganda. Her involvement aimed to represent the interests of sickle cell patients and the national anemia working group. Her efforts resulted in raising awareness of sickle cell disease, which had been overlooked for two decades. She then discussed barriers to patient involvement in regulatory activities, such as limited access to information, lack of representation, and inadequate resources for patient advocacy organizations. Identifying and addressing these barriers is crucial for fostering patient engagement. In her concluding remarks, Mukiibi offered tips for creating awareness among African patient communities about the importance of regulatory systems. These strategies involve community outreach, education, and collaboration with local healthcare providers.
Agenda
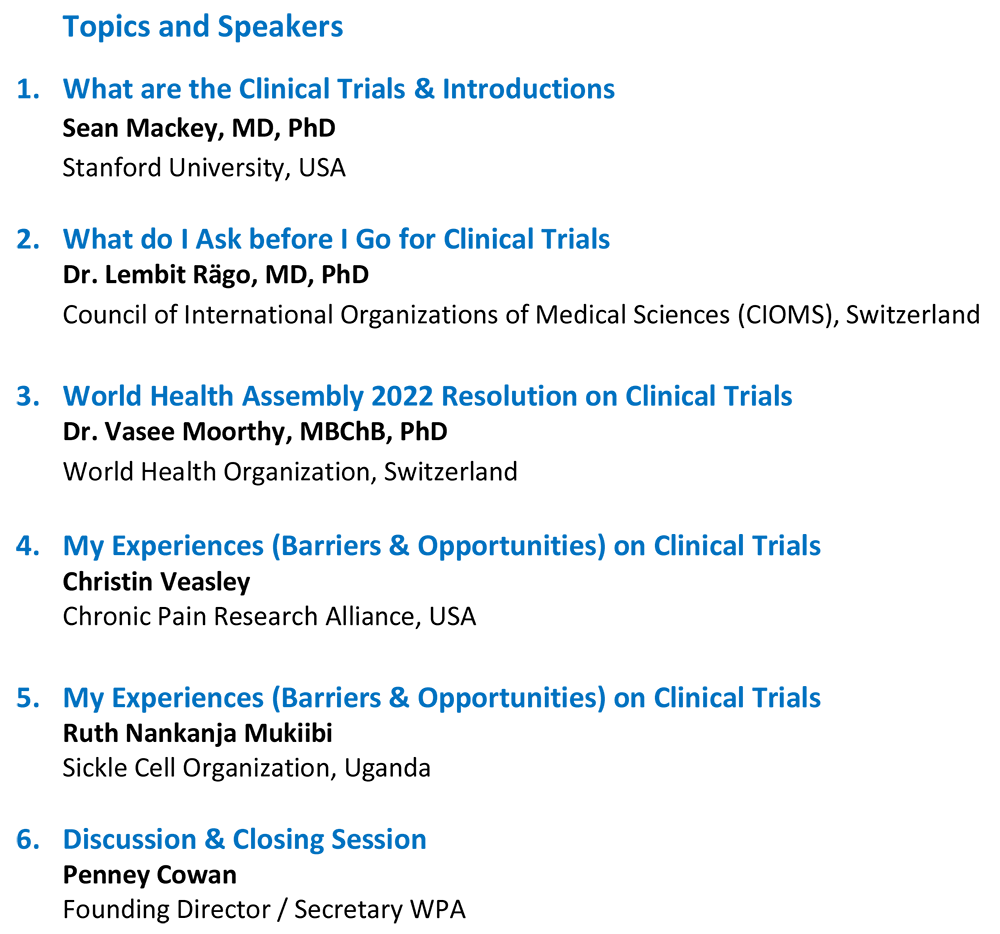
Speakers


• Founding Director of Sickle cell Association of Uganda (SAU) for last 23 years now. Sickle Cell Association of Uganda has so far reached out to more than 20 districts in Uganda and has a vast membership of patients and caregivers.
• Board Member at The Academy for Health Innovation, Infectious Disease Institute representing community perspective.
• Board member of the School of Biomedical Sciences Research and Ethics Committee, Makerere University Kampala.
• Member technical working committee for non-communicable diseases Ministry of Health Uganda (MOH).
• Member National Anemia Working Group MOH.
• Member National Steering committee for Sickle Cell Disease, MoH
• Representing the Association at community activities to enhance the organization’s community profile.




