- (000) 123 458 789
- office@worldpatientsalliance.org

PATIENT VOICES
Survivor Stories
Healing isn’t just about survival. It’s about purpose
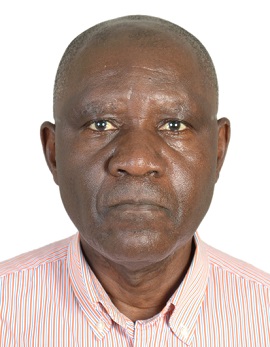
Joseph Rukelibuga
Stroke (Type2 Diabetes, Hypertension)
Rwanda
My name is Joseph Rukelibuga. I am a Rwandan with lived experience of Type 2 diabetes, hypertension, and stroke. I am a stroke survivor and the founder of Stroke Action Rwanda, the only stroke support organization in the country. Since 2019, I have been an active advocate for stroke patients. My storytelling usually includes three parts: my personal journey (the story of self), the experiences of fellow survivors (the story of us), and the urgent actions needed to address systemic gaps (the story of now).
My stroke occurred on June 20, 2016, at around 4:00 AM while I was at home. I was 57 years old at the time. Within an hour, my wife rushed me to the nearest referral hospital. A general practitioner administered an intravenous drip to bring down my dangerously high blood sugar and blood pressure. I was then admitted to a general ward with 15–20 other patients. We waited for a specialist—a kidney doctor who was on duty at another hospital—who arrived at around 9:00 AM. After examining me, he ordered further tests. The next day, on June 21 at 9:00 AM, I was diagnosed with an ischemic stroke with left-side hemiplegia, using ultrasonography of the carotid artery. Due to the delay in diagnosis and the unavailability of thrombectomy, I was prescribed aspirin cardio along with medications for diabetes and hypertension. Rehabilitation physiotherapy was recommended but not initiated until I was discharged from the hospital. I remained in the hospital for six days. Thankfully, my early arrival helped shorten my hospital stay.
In contrast, a colleague of mine who suffered a haemorrhagic stroke was not so fortunate. He arrived at the hospital 12 hours after his symptoms began because he was denied access to the only ambulance at his local health Center. Due to resource limitations, ambulances in Rwanda are prioritized for transporting pregnant women, to reduce maternal and infant mortality. My colleague stayed in the hospital for three months, developed aphasia, and after discharge received little follow-up care. He sadly passed away six months later.
Stroke patients in Rwanda are typically admitted to general internal medicine wards and treated by general practitioners. There are no dedicated stroke care units, and neurologists or neurosurgeons are very limited. Patients are often discharged once their vital signs stabilize, mainly due to overcrowded hospitals needing to make space for new admissions. Most patients are discharged without any assessment of their home environment, despite experiencing reduced mobility, speech difficulties, depression, or cognitive disorders. There is also a critical shortage of trained healthcare providers to support post-stroke rehabilitation. This makes the early post-discharge period especially dangerous for patients without trained caregivers. Falls are common and can lead to complications, including recurrent strokes. At the time of my discharge, neither I nor my family knew anything about stroke care or recovery. Information on stroke types, risk factors, disease progression, and secondary prevention was only provided much later by physiotherapists and cardiologists during medication refills.
Accessing quality and affordable rehabilitation services in Rwanda has been a serious challenge. Until recently, rehabilitation care was not officially included in the primary healthcare system. A few small private physiotherapy clinics exist in the capital, Kigali, but they do not offer occupational therapy, speech therapy, or neurorehabilitation. Most stroke survivors must pay out-of-pocket, and these services are very expensive. Although we have community-based health insurance, it does not cover private rehabilitation or certain essential medications.
Three weeks after my hospital discharge, I began attending regular physiotherapy sessions. Meeting other stroke survivors gave me emotional strength. Over time, I progressed—I eventually stood up from my wheelchair. After six months of consistent therapy, I returned to work. I worked for three more years before retiring. After retirement, I trained with the Our Views, Our Voices initiative of the Global NCD Alliance (NCDA) to become a lived experience advocate.
A combination of factors helped me recover aspirin cardio, diabetes and hypertension medications, physiotherapy, and peer support from other stroke survivors. However, I missed essential components of stroke care, such as thrombectomy, occupational therapy, and neurorehabilitation. Despite this, I consider myself fortunate to have survived and stayed mentally alert throughout my recovery. I remain deeply grateful to the healthcare providers who saved my life despite the very difficult working conditions they face.
Today, I call upon the Ministry of Health in Rwanda to establish stroke care units in referral hospitals and to distribute clear national guidelines for stroke care and treatment. We need more trained professionals and hospitals equipped to handle stroke cases, and we must invest in well-equipped post-stroke rehabilitation Centers at the community level. I missed critical elements of stroke care, but I stood up again—and today, I speak not just for myself, but for every stroke survivor still waiting to be seen, heard, and properly cared for.

