
WPSD Webinar: “Safe from the Start”: Patient Safety and Quality in Infant and Child
WPSD Webinar Report: “Safe from the Start” Patient Safety and Quality in Infant and Child Care
Date: September 9, 2025 • Organized by: World Patients Alliance (WPA)
Overview
WPA hosted a World Patient Safety Day webinar on the theme “Safe care for every newborn and every child.” The session spotlighted risks in neonatal and paediatric care and shared practical ways to reduce harm through safer childbirth, medication safety, diagnostic safety, and infection prevention. Participants could select their language via live interpretation. WPA reiterated its role as the world’s largest umbrella patient organization and noted growth to 700+ member organizations. (Transcript: welcome, multilingual access, membership update.)
Objectives
• Highlight distinct safety needs of newborns and children across care settings.
• Promote safe practices in childbirth, medication use, diagnostic processes, and IPC.
• Reinforce the importance of workforce training, family engagement, and system learning.
• Elevate caregiver and patient voices as drivers of safer care.
Speakers and Roles
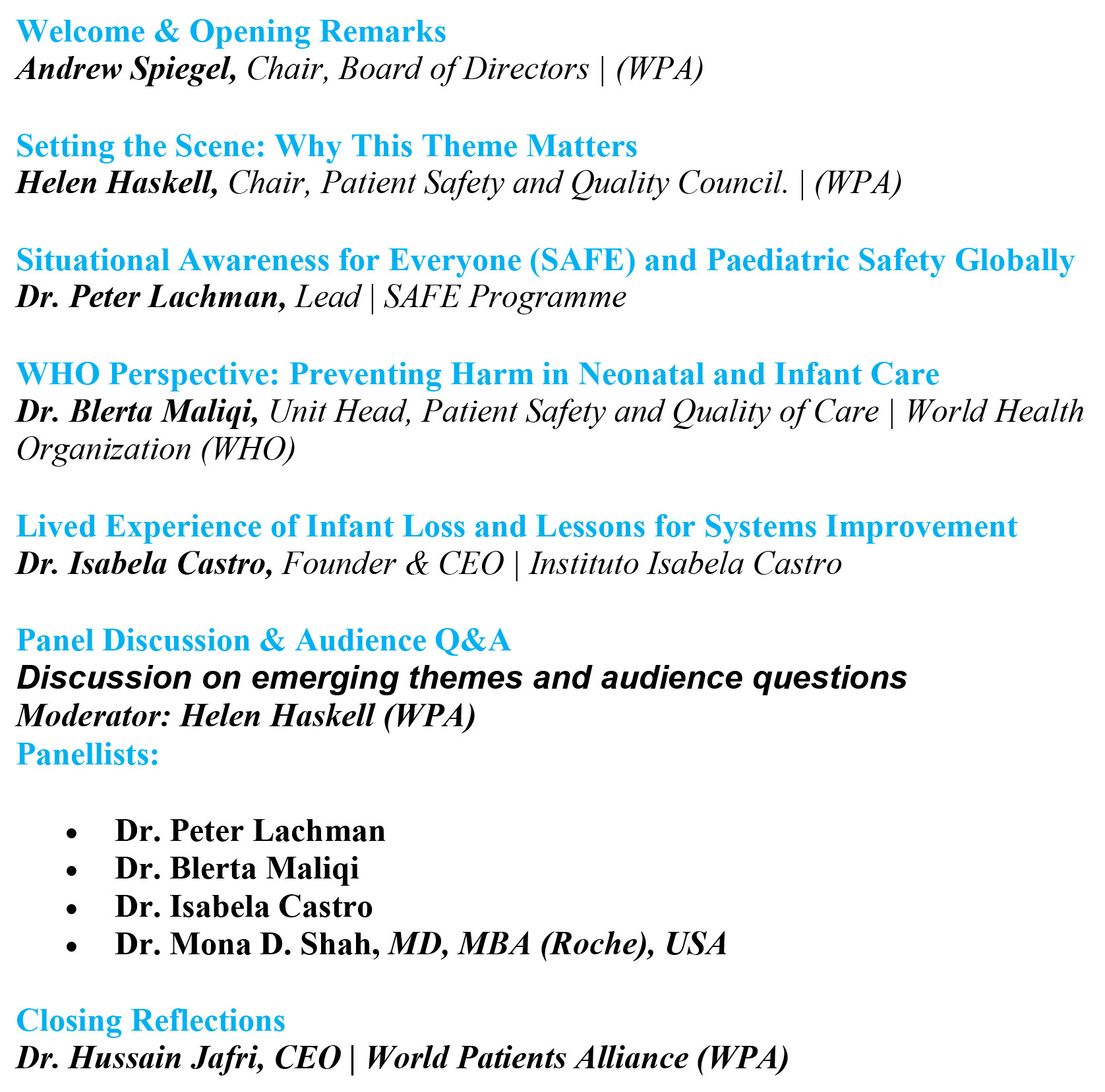
Highlights from Presentations
Setting the Scene (Helen Haskell)
• Framed “patient safety from the start” as a system and rights imperative.
• Introduced WPA resources for families: Patient Safety Books for Children, and the video “Children Are Not Little Adults” for paediatric safety awareness.
WHO Perspective, Preventing Harm in Neonatal and Infant Care (Dr. Blerta Maliqi)
• Recalled the scale of harm in paediatrics and neonatology.
• Emphasized potential to save 1 million newborns through improved quality of care.
• Urged adoption of WPSD 2025 goals, context adaptation, facility prioritization, teamwork culture, and measurement for improvement.
SAFE Programme, Situational Awareness for Everyone (Dr. Peter Lachman)
• Explained how team huddles, shared mental models, and real-time monitoring reduce harm.
• Described the medication-safety “Druggle” huddle and six safety questions adapted from Vincent to check current risk, recent harm, reliability of care, and future risk.
• Stressed psychological safety for parents to speak up and the co-production of care: “Services are based on relationships… equal partners co-producing health.”
• Shared a case where diagnostic anchoring to constipation missed a bowel volvulus, underscoring escalation and listening to families.
Lived Experience, Lessons for Systems (Dr. Isabela Castro)
• Shared the loss of her infant after unrecognized deterioration and limited family involvement.
• Called for transparent communication, timely escalation, and family inclusion throughout care.
• Highlighted the lasting emotional and professional impact, and how advocacy can drive system change.
Panel Discussion, From Principles to Practice
Family Engagement: Parents as partners in bedside ID checks, medication verification, and hygiene practices; build psychological safety so families can say “something’s not right.”
System Enablers: Trained staff, reliable supplies, standard protocols, and non-punitive reporting that drives learning.
Measurement: Track adherence to safe-birth bundles, paediatric medication processes, IPC indicators, and parent-reported experience measures.
Equity: Focus on low- and middle-income settings where risks and infection burdens are higher.
Key Takeaways
Start safety at birth. Neonatal care needs vigilant teams and family inclusion.
Strengthen teams. Situational awareness and structured huddles reduce preventable harm.
Engage families. Psychological safety enables parents to contribute critical insights.
Build systems that learn. Standardize, measure, and act on what the data and families tell you.
Acknowledgments
WPA extend our deepest gratitude to Roche for their generous sponsorship of the World Patient Safety Day 2025 Campaign, which enables us to advance this vital mission.
Speakers



Mona D. Shah, MD is a paediatric haematologist-oncologist, who earned her MD degree at the University of Maryland in 2001. She completed both her categorical paediatrics and global health residencies in 2004, followed by a paediatric hematology-oncology fellowship in 2007. She earned her MS in Clinical Investigation as part of the Clinical Scientist Training Program (CSTP) at Baylor College of Medicine in 2011, and more recently, completed an Executive MBA at Rice University Jones School of Business in 2018. Dr. Shah was an Associate Professor at Baylor College of Medicine (2007 - 2020) in both Paediatrics and Medicine, local site PI on a number of paediatric haemostasis/thrombosis clinical trials, and spent 10 years as an Associate Medical Director of Clinical Operations, Quality, and Safety at Texas Children’s Hospital, Houston, TX. Dr. Shah joined Genentech (a Member of the Roche Group)’s Product Development - Oncology-Hematology in February 2020, quickly advancing to Lead Medical Director, where she served as Medical Monitor for 2 Phase III clinical trials (crovalimab in atypical haemolytic uremic syndrome). She was also engaged with the Renal Franchise in developing crovalimab in lupus nephritis (Phase I & II clinical trials in development), and with the Human Factors/Paediatric Formulations Working Group on autoinjector devices and oral formulations for children. After completing a rotation in Early Development Safety (EDS), she was promoted to Senior Medical Safety Director in Late-Stage Marketed Medicines Safety and was appointed Safety Strategy Lead for giredestrant in early and metastatic breast, ovarian, and endometrial cancer global clinical trials. She has experience in innovative study designs (adaptive/multi-drug), with FDA/EMA paediatric investigational plans, and health authority interactions. In June 2023, she was appointed Paediatric Safety Lead, in collaboration with the innovative Paediatric Oncology Drug Development (iPODD) Team, supporting safety for paediatric indications and devices, and serves as the Co-Chair of the Paediatric Safety Expert Group at Roche. Since July 2022, she also joined Stanford University School of Medicine, as an Adjunct Clinical Associate Professor in the Department of Paediatrics, Division of Hematology-Oncology, where she enjoys teaching MSII students, and at the bedside in the Lucille Packard Bass Center Clinic.


Peter Lachman works across different countries. In Ireland he has delivered programmes to develop clinical leaders in quality improvement at the Royal College of Physicians of Ireland. In Africa he has delivered patient safety and quality programmes in Sudan, Tanzania, Ethiopia and Mozambique for the Health Service Executive (HSE) Global Health Programme. He is the Director of the Patient Safety Movement Foundation Kiani Global Interprofessional Patient Safety Fellowship. He was Chief Executive Officer of the International Society for Quality in Healthcare (ISQua) 2016 -2021. He was a Health Foundation Quality Improvement Fellow at Institute for Healthcare Improvement in 2005-2006, Deputy Medical Director (Patient Safety) at Great Ormond Street Hospital and Consultant Paediatrician at the Royal Free Hospital 2006-2016; and North West London NHS Trust at Northwick Park Hospital 1996-2004. Previously he was a consultant paediatrician in Cape Town at the Red Cross War Memorial Children’s Hospital. He is the lead editor of the OUP Handbook on Patient Safety published in April 2022; co-editor of the OUP Handbook on Medical Leadership and Management published in December 2022; and editor of the OUP Handbook on Quality Improvement in Healthcare published February 2024.

Dr. Blerta Maliqi is a global health leader with three decades of experience advancing health systems strengthening, policy development, and service delivery, with a strong focus on quality of care and patient safety. As Unit Head at the World Health Organization (WHO) in Geneva, she leads efforts to ensure safer, more effective, and people-centered health services worldwide. Throughout her career, she has played a pivotal role in shaping global health strategies and supporting countries to translate policies into action. She has provided strategic leadership in advancing global health priorities, helping countries strengthen policies, improve services, and enhance accountability for results, particularly in the area of maternal and child health. Among her key contributions, Dr. Maliqi has led global initiatives to improve the quality of care for maternal, newborn, and child health, working closely with governments, frontline health workers, and international partners to embed quality standards, strengthen service delivery, and drive better health outcomes. A strong advocate for collaborative action, Dr. Maliqi has been instrumental in developing innovative tools, authoring global reports, and producing implementation guidance that continue to influence health policies and practices worldwide. She holds a Medical Degree, a Ph.D. in Health Systems Management, and a Master’s in Health Management, Planning, and Policy.

